Psychosocial well-being after stroke: Our research approach
Grounding our research in the needs and perspectives of people living with stroke and health care professionals
In developing this proposal, we met with clinicians, stroke survivors and their whānau, to explore what they saw as priorities for this research. Everyone agreed that psychosocial well-being and psychosocial care is often invisible and undervalued. They want this research to make psychosocial well-being and psychosocial care visible and valued.
Stroke whānau want to be recognised as key in supporting well-being and want knowledge and resources to do this. They want strengths-based services that are holistic and wairua-centred. Clinicians want to be more confident and supported in providing this care, and in advocating for this approach to managers and funders.
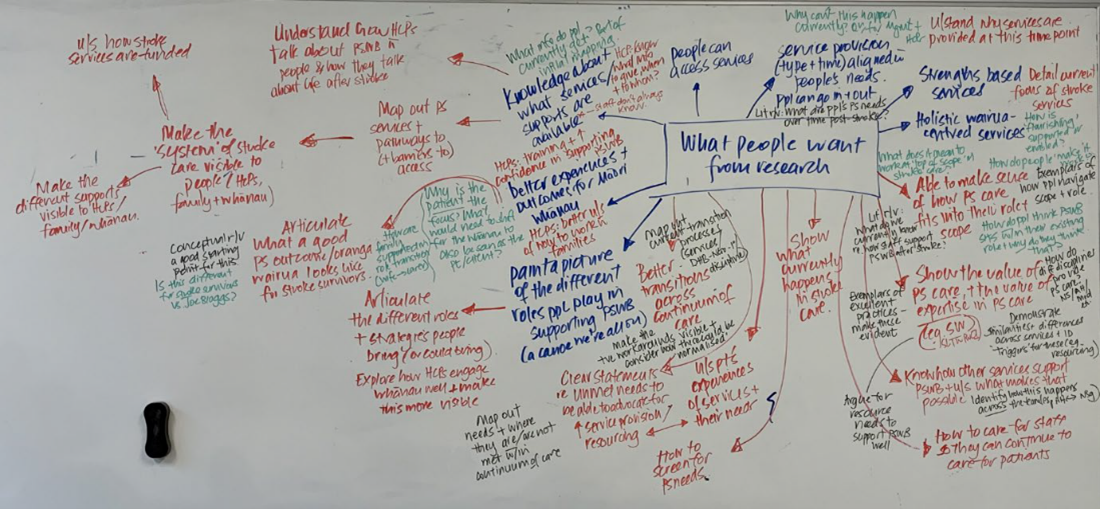
Summary of our discussions with stakeholders
The summary of these discussions, and our considerations of how this might inform our research process and products, can be found here.
He Awa Whiria: Valuing Māori and non-Māori knowledges
Our research approach is based on He Awa Whiria—Braided Rivers Model. In this, Māori and non-Māori knowledges are uniquely engaged with, and considered together at different points throughout the research process. This approach enhances understandings but ensures each stands in its own right.
Utilising He Awa Whiria is one way we are honouring our responsibilities under Te Tiriti o Waitangi. Māori and non-Māori experiences, perspectives and knowledges hold equitable value and privilege. We acknowledge mātauranga Māori as its own interwoven form of knowledge that is critical for ensuring research and resulting practice recommendations are Māori centred, reflect Māori aspirations and contribute meaningfully toward achieving health equity for stroke whānau.

A multi-staged research approach
Our research has a number of different components to it.
In the first stage of research, we are undertaking literature reviews to understand how psychosocial well-being is experienced after stroke in Aotearoa New Zealand. Whilst our study is based on Kirkevold’s definition of psychosocial wellbeing1, this is generated from international theory and evidence. Our reviews centre on ‘what do people living with stroke tell us about what constitutes psychosocial well-being in Aotearoa New Zealand’ and this knowledge is used to refine and challenge Kirkevold’s definition, to produce a definition/s and terminology that is specific and culturally appropriate for use in Aotearoa New Zealand. This then underpins our ongoing work programme.
One review explores how Māori stroke survivors and whānau experience psychosocial well-being after stroke. We conduct a secondary analysis of qualitative studies of Māori stroke survivors and whānau from Aotearoa New Zealand, as well as other forms of knowledge such as material on television, in magazines, or in theses.
The other review examines how psychosocial well-being is conceptualised in the published stroke literature in New Zealand. We conduct a secondary analysis of qualitative studies of stroke survivors’ experiences of life after stroke, drawing on literature published from research in Aotearoa New Zealand.
Following this, we will conduct a metasynthesis of published qualitative reviews that examine how stroke survivors and whānau perceive their psychosocial well-being was addressed within care in Aotearoa New Zealand and internationally. We will use a Framework approach to data synthesis2, drawing on our framework/s of psychosocial well-being constructed in through the earlier literature reviews.
- Kirkevold M, Bronken BA, Martinsen R, et al. Promoting psychosocial well-being following a stroke: developing a theoretically and empirically sound complex intervention. Int J Nurs Stud 2012;49(4):386-97. doi:10.1016/j.ijnurstu.2011.10.006
- Flemming K, Noyes J. Qualitative evidence synthesis: Where are we at? IJQM 2021;20:1609406921993276. doi: 10.1177/1609406921993276
Full details of the review protocol can be obtained from our team. Please email us on: wellbeing.study@aut.ac.nz if you would like more information.
To gain a deeper understanding of how psychosocial well-being is addressed and experienced within stroke care in Aotearoa, we will speak with stroke survivors and whānau, stroke practitioners, and expert informants with specialist understandings of the stroke context. Through these conversations we hope to understand how psychosocial well-being is experienced by stroke survivors and their whānau. We also want to know how it is addressed within care from the perspectives of clinicians, service managers and stroke leaders. Finally, we hope to gain insight into how care practices are shaped by the practice context.
We will engage with participants through individual interviews, focus groups, and wānanga to hear their perspectives. We will specifically seek to engage with both Māori and non-Māori stroke survivors, whānau, practictioners, and expert informants, under the guidance of the Māori and non-Māori research stream leads respectively. Throughout the research we will connect with participants regularly so they are kept up-to-date with progress, and have the opportunity to provide feedback.
In addition to the insights shared by participants, we will also examine texts (documents) which shape practice (for example, guidelines and policies). Together, this data will allow us to gather rich nuanced understandings of which care practices and processes support psychosocial well-being at different stages of stroke care, and which may be most amenable or most important to change if we are to enhance psychosocial wellbeing.
As we gain a greater understanding - both of what people think is working well, and what could be done differently - to support well-being of stroke survivors and whānau, we will take our research back to those who have been involved to explore their priorities for change. We will work together with stroke survivors and whānau, stroke practitioners and service leaders to co-design and produce resources that enhance practitioner and service capability to support psychosocial well-being after stroke. The exact nature and focus of this process will be dependent on findings from the earlier stages of the research.
Psychosocial well-being after stroke
Supporting well-being after stroke to improve understanding and enhancing care.